Ovary
#61 Ovary
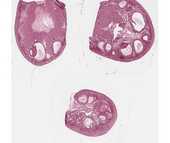
There are 3 sections of ovary on this slide. At low power note the general division of the ovary into an outer cortex containing follicles in various stages of development and an inner medulla containing numerous blood vessels and dense fibrous connective tissue.
Identify:
- Lining epithelium (classically called "germinal epithelium") - a simple cuboidal covering the ovary, continuous with the mesothelium of the peritoneum.
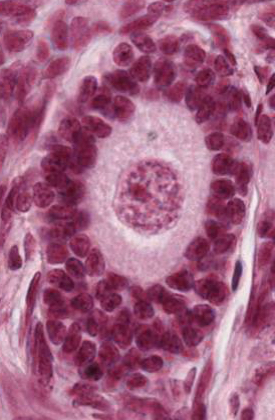
- Primordial follicles - 1o oocytes surrounded by a single layer of squamous granulosa cells. This is a resting stage.
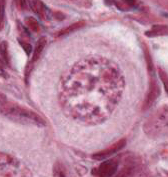
- Primary follicle - 1o oocyte surrounded by cuboidal or columnar granulosa cells, first as a single layer, and then multi-layered. Theca forms outside the basal lamina of the granulosa cells. Zona pellucida surrounds oocyte. These are growing follicles.
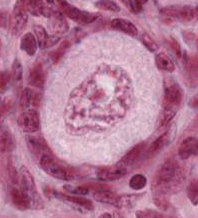
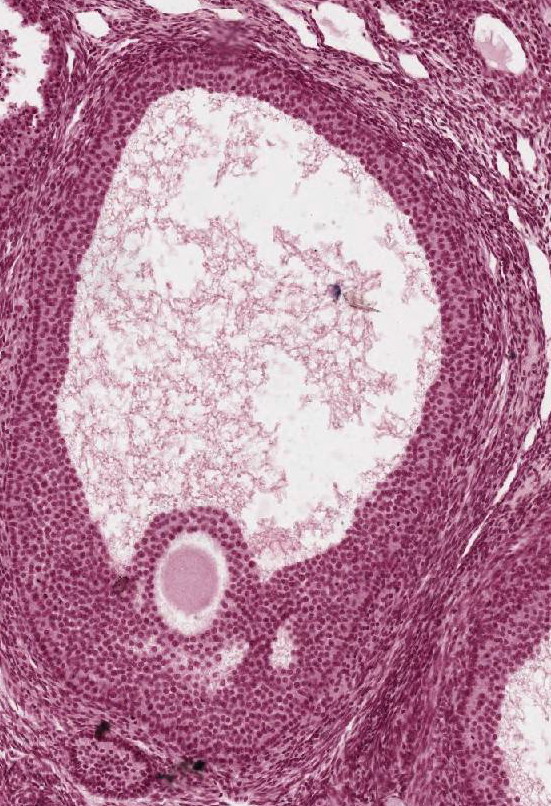
- Secondary (antral) follicles - 1o oocyte surrounded by granulosa cells among which fluid-filled spaces are coalescing into a single space, or antrum. Outside the basal lamina of the granulosa layer, the theca has differentiated into a theca interna and a theca externa.
- Mature preovulatory (Graafian) follicle - characterized by a very large, central antrum. Zona pellucida is very conspicuous. 1o oocyte is surrounded by a layer of granulosa cells (the corona radiata) and rests on a small mound of granulosa cells called cumulus oophorus.
- Atretic follicles - Note that follicles may undergo atresia during any stage of development. Atresia is often first recognized in the granulosa cells; the nuclei become apoptotic and there is a loosening of the cells.
- Corpus luteum - Following ovulation follicular cells (both granulosa and luteal) fold into the empty follicle and undergo luteinization. Following fertilization the corpus luteum becomes a large, steroid-producing organ.
- Corpus albicans - If fertilization does not occur, the corpus luteum regresses. The corpus albicans is the connective tissue scar remaining from a degenerated corpus luteum.
#63 Ovary, Adult Human, H&E
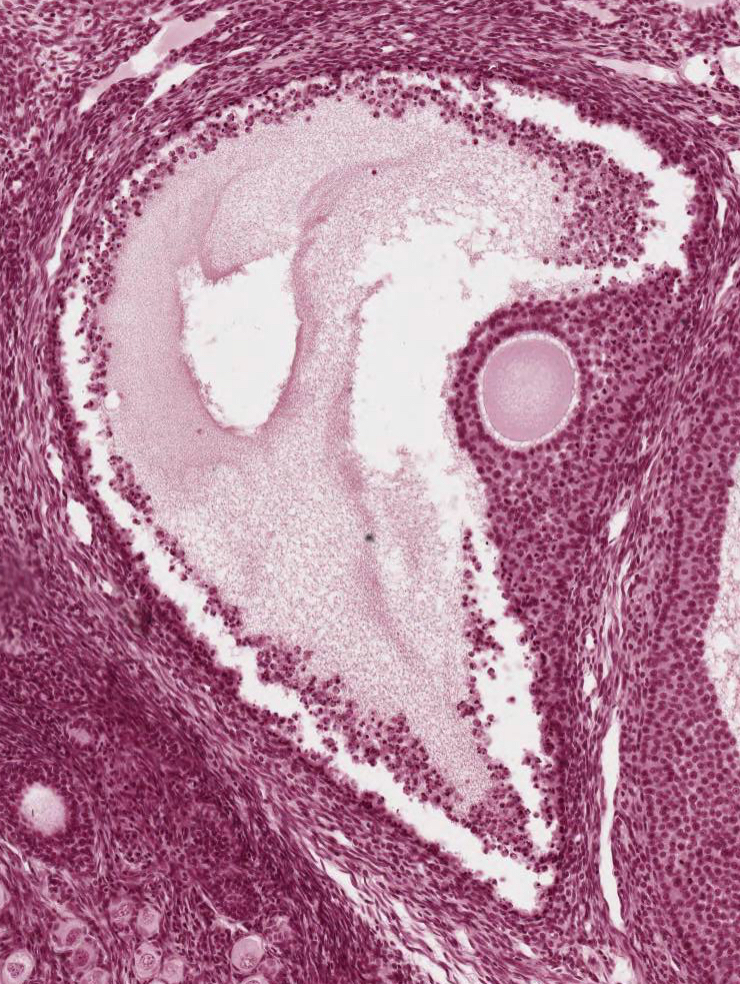
Note the scarcity of primary follicles, suggesting that this ovary is from an older woman. Identify a corpus albicans (the connective tissue scar remaining from a degenerated corpus luteum).
 This section contains a recently formed, corpus luteum that dominates the ovary. Notice the folding of its wall and the large central cavity filled with coagulum. Identify the two primary cellular components of the corpus luteum: the granulosa lutein and theca lutein cells. Notice the relationships of these two cell types to each other and to the vascularization of the developing corpus luteum. The theca lutein cells follow the pathways of the invading blood vessels.
This section contains a recently formed, corpus luteum that dominates the ovary. Notice the folding of its wall and the large central cavity filled with coagulum. Identify the two primary cellular components of the corpus luteum: the granulosa lutein and theca lutein cells. Notice the relationships of these two cell types to each other and to the vascularization of the developing corpus luteum. The theca lutein cells follow the pathways of the invading blood vessels.
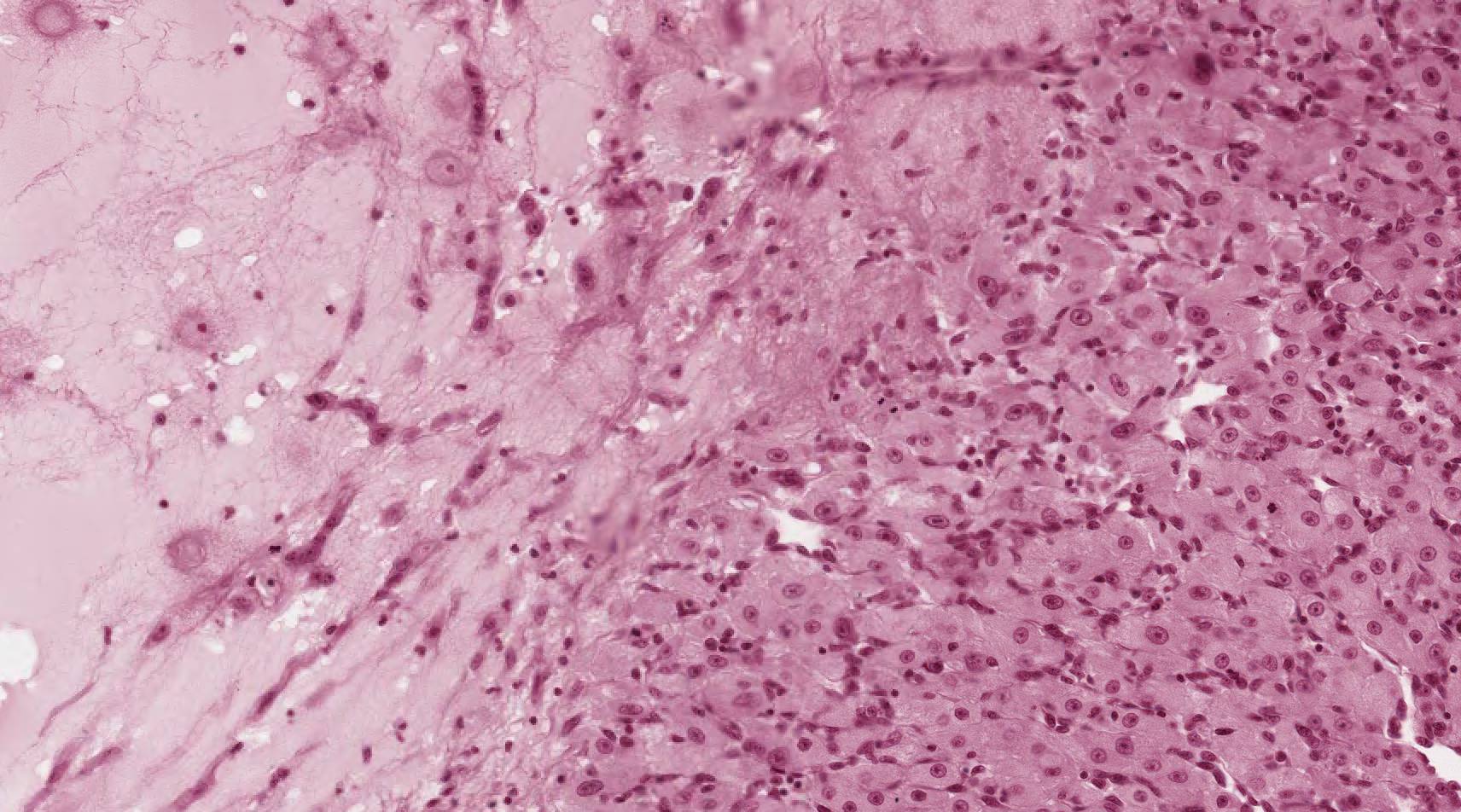
#64 Ovary, Corpus Luteum of Pregnancy
Compare the development of this corpus luteum of pregnancy (probably from the first trimester) with that of the recently formed corpus luteum of slide #63. Note particularly the increase in thickness of the granulosa luteal layer as compared to the thin, peripheral zone of theca luteal cells. The extensive vacuolization of the granulosa luteal cells is due to the extraction of its abundant lipid droplets. This reflects the importance of the corpus luteum (particularly the granulosa lutein cells) as the primary ovarian source of the steroid hormone progesterone.
What is the primary ovarian source of estrogenic hormones?
What are the fine structural specializations of ovarian cells involved with the production of steroid hormones?
Be certain that you understand the changes that occur within the follicle during follicular development.
Consider the hormones of the anterior pituitary involved in follicular growth and ovulation.